New corona virus Covid-19 poses a few problems for the professional launderer, writes LTC’s Richard Neale who has compiled essential information and guidelines for dealing with the virus for laundries and linen rental businesses
We are witnessing the outbreak of a novel, and occasionally lethal, corona virus of the family that includes SARS (severe acute respiratory syndrome) and MERS (Middle Eastern respiratory syndrome). The outbreak centres on Wuhan, China, but has spread rapidly to cause multiple infections in several countries and more than 3,884 deaths so far, at the time of writing (March 9).
We look at how the professional launderer and textile rental operator can cater for the risks associated with this outbreak and minimise its potential to affect staff and customers.
What exactly is the new virus?
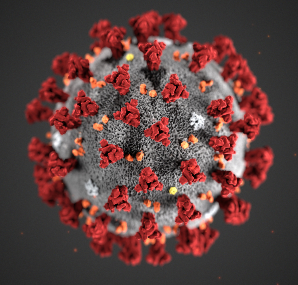
The virus has been widely referred to as WN-CoV (Wuhan corona virus), but the World Health Organisation (WHO) have named officially as Coronavirus Covid-19. It is one of the family of corona viruses, which includes the common cold. It is a physically large virus, typically about 0.125 micron across with a surface covered by spiky projections, making it too large to survive or stay suspended in air for very long or to travel more than a few metres (1).
Corona viruses have an incubation period and the time delay from infection to symptoms with the new bug is not known. The longer it is, then the greater the likelihood of epicentres developing around some of the travellers who have returned from an affected country to their home countries. If each infected traveller is infecting two or three more people, then there will be a steep initial increase in cases, much like the one currently being reported for Wuhan. Although there are other factors at play (such as the speed and magnitude of the official response), it does appear that the increase in cases of Covid-19 in 2020 is much steeper than for SARS in 2003.
Corona viruses in general are very susceptible to destruction at elevated temperatures. However, Covid-19 appears to be much more resistant to thermal destruction and research work in Germany suggests that to kill it requires either 10 minutes at 90C or 15 minutes at 85C, plus mixing time in both cases. This is well in excess of the normal 71C for 3 minutes widely used in healthcare.
It is advised (3) that the new corona virus can be effectively removed from surfaces by wiping with an EPA-approved disinfectant such as sodium hypochlorite at a concentration of 950ppm or 0.1%. This is much stronger than the bleach rinse in the UK Department of Health advice to launderers, which calls for a rinse concentration of 150ppm sodium hypochlorite (4).
How can the professional launderer best guard against the risks posed by the new virus?
Work using Murine Parvovirus has shown that this organism is even more resistant to thermal destruction than Coronavirus Covid-19. It has therefore been used as a reference virus and assumed that if a process kills this virus it will also deal effectively with Covid-19.
Raising main wash temperatures to cope with Covid-19 by implied thermal disinfection would work, but it will greatly increase the carbon footprint of the laundry. This is unfortunate because it risks reversing the recent trend towards low temperature washing across the professional laundering sector. Increasing main wash temperatures up to 85 - 90C for 10 – 15 minutes plus mixing time would increase significantly the energy consumption of the washhouse, when many are working successfully at 40C.
However, the Coronavirus Covid-19 is susceptible to thermo-chemical disinfection, so if the laundry practising low temperature washing is also using chemical disinfection (as it should be), then this could be arranged to deal with the new virus. The most successful approach looks to be one of the new processes based on peracetic acid and leading suppliers offer a variety of time/temperature/chemical combinations, at temperatures mainly from 55 to 70C. Many of these have been independently certified as effective by the Robert Koch Institute (RKI) in Germany.
Suggested procedures to be followed
This leads us directly onto the procedures that need to be adopted in the commercial and healthcare laundry to deal with the outbreak. The following systematic approach is recommended until official guidance is published:
Boxout
• Start implementing the necessary procedures straight away – do not delay. There is a risk of rapid increase in cases involving Covid-19 in every country to which travellers from affected countries have recently returned and this should be addressed quietly and competently now.
• Work from customers not known to be affected by the virus should be accepted in the normal way, but it should be processed as described in the following paragraphs to minimise the unintentional spread of disease from the occasional infected person who is not yet aware of this.
• Collection staff/drivers should be issued with gloves that are either washable or disposable and instructed to wear them whilst at work. This will provide first line protection against chance infection from contaminated surfaces at customer sites and on laundry bags. Eating and drinking whilst on collection duties should not be permitted.
• If cases of Covid-19 are reported in the country of operation, then protective wear should be uprated to include face masks and goggles or face shields. Both of these should be capable of close fitting to the wearer’s face to avoid ingress via gaps at nose, mouth or eyes. Even then the protection they provide is limited, but much better than nothing. An N95 mask is better than a paper one (because if correctly fitted it removes 95% of particles/aerosols), but a paper one is probably better than no mask at all.
• Sorting staff and washhouse operatives should be issued with washable gloves and goggles/facemasks straight away and should have priority for N95 masks when available, because they have to handle and move every incoming item, so are much more at risk than drivers. Covid-19 is frequently an airborne virus.
• Ventilation in the sorting room should be turned on and arranged so that clean air is drawn towards the sorting staff and contaminated air, from above the work being sorted, is drawn away from the sorters.
• Wash programmes should be overhauled and re-designed where necessary (in conjunction with chemicals suppliers) to assure disinfection from both bacteria and viruses (including Covid-19), either by implied thermal means or thermo-chemically. Chemicals suppliers will generally have much more information than is generally available, from their initial research and proving trials when they formulated and certified their processes. For the avoidance of doubt, disinfection must be achieved in the wash process, with no reliance on the heat in downstream finishing operations, because despite the apparent high temperatures in finishing, these have been shown not to be effective in achieving disinfection. (In some early work by LTC, 22 minutes in a tunnel finisher at a temperature of 150C still allowed enough bugs to germinate in the seams of a workwear garment to create a foul stench on the clean garment within three days.)
• Particular care is then needed to prevent re-infection of the clean items, which could occur from the outside of a washer extractor which was not wiped down with disinfectant (e.g. 950ppm sodium hypochlorite) after last being loaded. Transmission could occur if the clean items, even when wrapped, are allowed near the sorting area. If an infected operative or driver coughs or sneezes onto a batch of clean items, that would probably be sufficient to transfer to a customer handling the goods. The virulence of this particular virus looks likely to be sufficient then to precipitate further onward transmission.
• Every member of staff, visitors and contractors should be encouraged to wash their hands frequently, especially before eating or drinking. Staff should be shown the approved hospital method for handwashing and persuaded to adhere to it.
• Staff should wear a protective coverall and this should be laundered frequently and not be taken home.
All of these precautions will look very familiar to laundries currently handling healthcare work. It is quite reasonable to draw the conclusion that every healthcare provider working to the latest version of European Standard EN14065 will be effectively killing bacteria with a reduction of 5log10, but this is unlikely to deal with Covid-19. This virus will need either an increase in the time/temperature in the main wash or a certified thermo-chemical disinfection process. In addition, there is a more widespread need for eye, nose and mouth protection. This should be heeded as a precaution to prevent the spread of Covid-19 amongst commercial and healthcare customers.
In the less likely event of a more widespread epicentre of the epidemic developing in a country, with cases numbering in the tens of thousands, then more will be needed. The precautions already listed should have already been instituted and it is recommended that the effectiveness of these be cross-checked using the laboratory facilities of chemicals suppliers, microbial specialists and local technical service companies. It is expected that a rapid test for Covid-19 will quickly become much more widely available, which will help matters considerably. Laundries may then wish to obtain copies of the certification for the processes they are using, providing assurance that it is sufficiently effective against Covid-19 and so discharging their duty of care.
Conclusion
If the laundry and textile rental sector responds swiftly and expertly to the advice in this article then the likelihood is that the virus will be brought quickly under control, with very few new centres of significant infection. However, it is not going to disappear in the short term and the worst risks to the sector are only going to be realised if laundries do nothing to address them.
IMAGE: Courtesy of Centers for Disease Control and Prevention (CDC) Public Health Image Library
References:
• Icahn School of Medicine, Department of Public Health Science.
• Chan K H et al: Hindawi Open Access: Advances in Virology: Volume 2011 Article ID 734690.
• CDC advice issued by the US Centers for Disease Control.
• UK Department of Health Guidance Note HSG(95)18 – Hospital laundry arrangements for used and infected linen.